Despite advances in treating inflammatory bowel disease (IBD), there is still a need for safe and effective therapies that can induce and maintain remission in a larger proportion of patients. Each individual with IBD is unique, and a personalized approach to treatment is highly desirable due to the diverse nature of the disease.
Exciting research is currently underway, led by Dr. Derek McKay and his team at the University of Calgary. The study aims to explore the potential use of a patient's own immune cells to combat the symptoms of inflammatory bowel disease (IBD) and promote healing of the gut. Immune cells, which are the body's natural defense system, help protect us from harmful substances and fight off infections. One type of immune cells called macrophages is at the center of this ground-breaking research. These remarkable cells have the ability to target and alleviate the symptoms of IBD through the action of a natural, anti-inflammatory molecule. By leveraging the patient’s own immune system, Dr. McKay's innovative approach has the potential to revolutionize IBD treatment, offering new hope and possibilities for individuals with IBD.
To decipher the role of macrophage-driven therapies, the team first isolated macrophages from healthy donors to investigate how these cells respond to interleukin 4 (IL4), an immune-signaling molecule. Immune-signaling molecules are substances that help regulate immune responses and communication between immune cells. Specifically, IL4 is known to repress inflammation, and thus, is an ideal candidate for personalized therapy development. To test if IL4-treated macrophages exhibit healing properties, the researchers conducted a wound-healing assay. This experiment consists of simulating a wound to a layer of intestinal cells in a lab dish in the indirect presence and absence of IL4 treated macrophages.
(Figure 1)
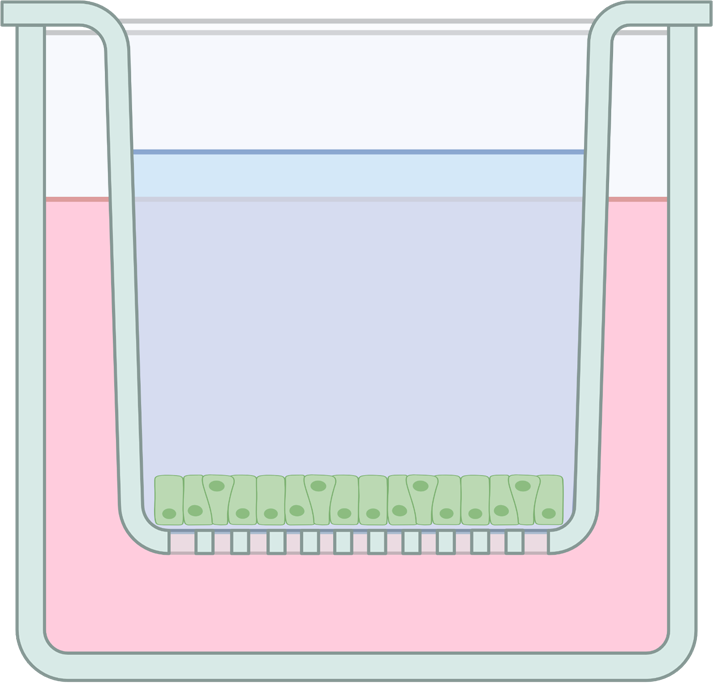
Researchers grow intestinal cells in a small dish
Researchers make a small "wound" or gap in the cells
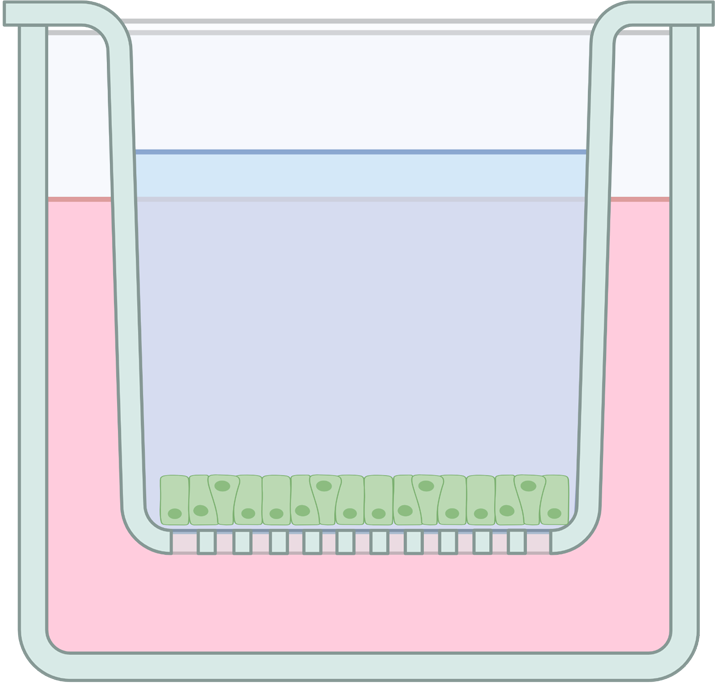
Researchers treat macrophages with IL4 and expose the "wound"
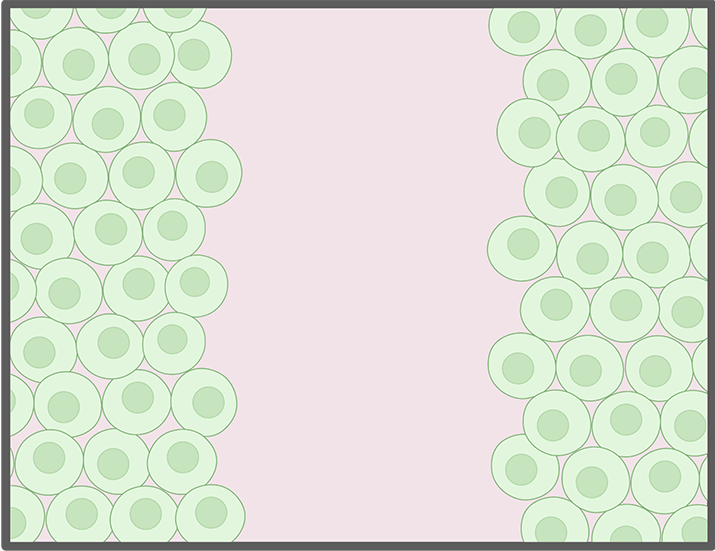
Figure 1 (Top panel): In a wound healing assay, researchers grow a layer of intestinal cells (in green) in a dish. They induce a small wound and test if exposure to different conditions (e.g. IL4-treated macrophages) promote healing of the induced wound.
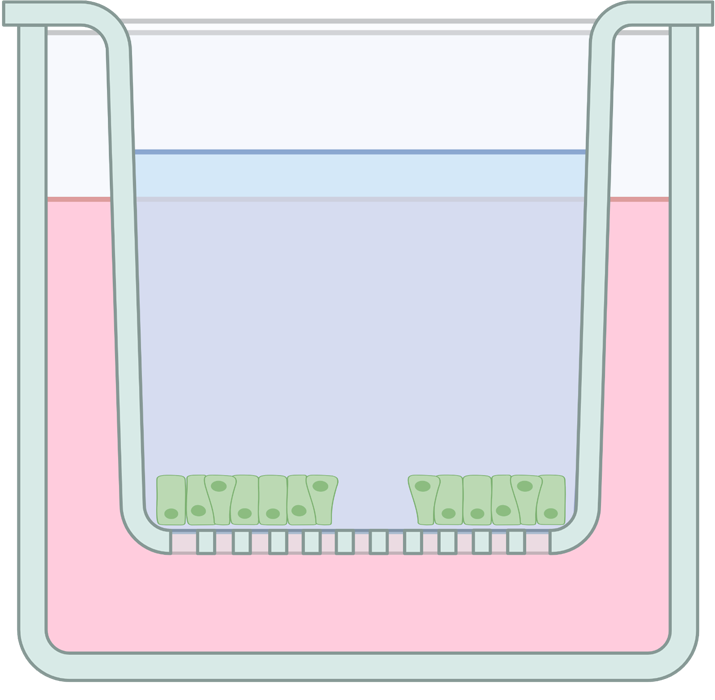
(Figure 2)
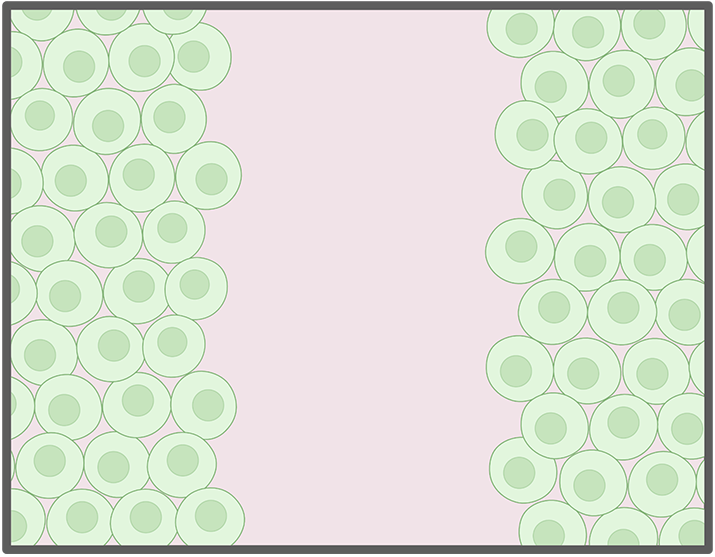
"induced wound"
Exposure to IL4 treated macrophages healed the wound.
"induced wound"
...While exposure to non-treated macrophages did not.
Figure 2. (Bottom panel): The McKay Team observed the induced wound was healed when exposed to IL4-treated macrophages (in darker blue), but no healing effect was observed when exposed to untreated macrophages (in lighter blue).
The results of the study were highly promising. Macrophages treated with IL4 released specific molecules that exhibited pro-healing and anti-inflammatory effects, surpassing the performance of macrophages without IL4 treatment. Furthermore, in mice with IBD, those receiving IL4-treated human macrophages showed significantly improved disease outcomes compared to those receiving a placebo.
While this research is ground-breaking, it's essential to consider potential risks, such as the impact of immunosuppressive macrophages on cancer development.
Dr. McKay's study serves as a critical foundation for the development of personalized therapies that harness the power of a patient's own cells to combat IBD symptoms and promote healing.
In conclusion, Dr. McKay's research paves the way for a new era of personalized therapy for people with Crohn’s or colitis. By leveraging our own immune cells, we have the potential to alleviate symptoms, enhance healing, and improve the overall quality of life for those affected by this condition. With continued exploration and advancements, we can look forward to brighter prospects in finding the cures for Crohn’s and colitis.
To access the original published story, please visit frontiersin.org.